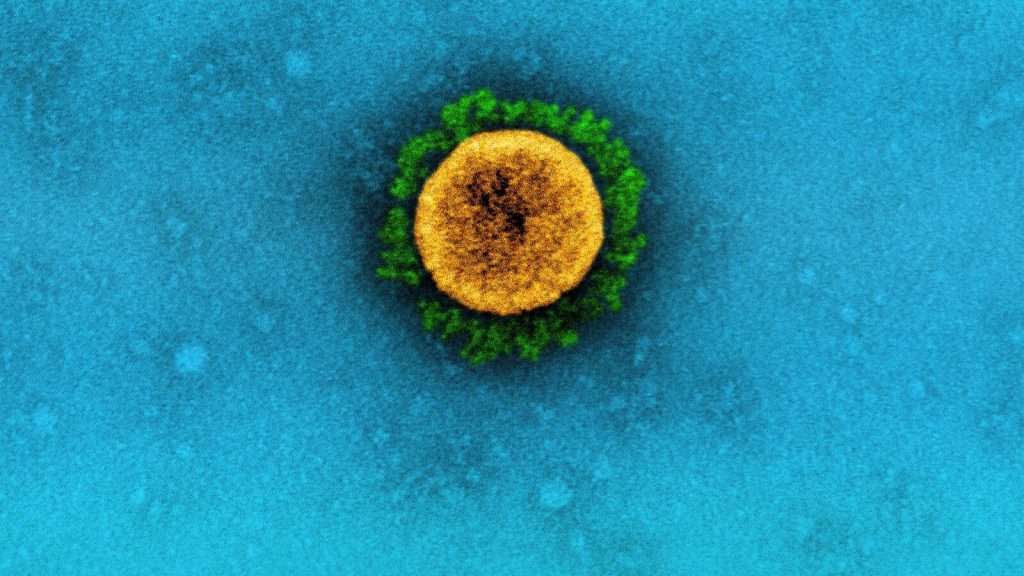
More than five years after the first cases of COVID-19 were detected in the United States, hundreds of people are still dying every week.
Last month, an average of about 350 people died each week from COVID, according to data from the Centers for Disease Control and Prevention (CDC).
While high, the number of deaths is decreasing and is lower than the peak of 25,974 deaths recorded the week ending Jan. 9, 2021, as well as weekly deaths seen in previous spring months, CDC data shows.
Public health experts told ABC News that although the U.S. is in a much better place than it was a few years ago, COVID is still a threat to high-risk groups.
“The fact that we’re still seeing deaths just means it’s still circulating, and people are still catching it,” Dr. Tony Moody, a professor in the department of pediatrics in the division of infectious diseases at Duke University Medical Center, told ABC News.
The experts said there are a few reasons why people might still be dying from the virus, including low vaccination uptake, waning immunity and not enough people accessing treatments.
Low vaccine uptake, waning immunity
During the 2024-25 season, only 23% of adults aged 18 and older received the updated COVID-19 vaccine as of the week ending April 26, according to CDC data.
Among children, just 13% of them received the updated COVID vaccine over the same period, the data shows.

This photo shows a vial of the Moderna Covid-19 vaccine, Bivalent, at AltaMed Medical clinic in Los Angeles, Oct. 6, 2022.
Ringo Chiu/AFP via Getty Images
Dr. Gregory Poland, a vaccinologist and president and co-director of the Atria Research Institute — which focuses on disease prevention — said there are likely not enough people receiving the vaccine, which is contributing to the number of weekly COVID deaths.
However, for those who have received the vaccine, some may not be developing a proper immune response.
“There are some people who may be genetically inclined to not respond well to the vaccine. That’s the topic I have studied with other viral vaccines,” Poland told ABC News. “The more common issue is that people are immunocompromised and can’t respond well.”
Additionally, Poland said that immunity from COVID-19 vaccines wanes over time, increasing the likelihood of being infected.
This is why the current recommendation for those aged 65 and older is to receive two doses of the updated COVID vaccine six months apart.
“Another reason for death due to COVID is being elderly, being what we call immunosenescent, where you do not have the immunologic ability to respond the same way you did in your 30s and 40s,” Poland said. “On top of it, if you do get infected by the time you’re in your 70s, 80s, there is some … accumulating co-morbidity.”
CDC data shows that those aged 75 and older currently have the highest rate of COVID-19 deaths at 4.66 per 100,000.
Not accessing COVID treatments
Currently, there are treatments for COVID-19 patients in the form of antiviral pills, including molnupiravir from Merck and Ridgeback Biotherapeutics and Paxlovid from Pfizer.
Both treatments must be started within five days of COVID symptoms appearing and are given twice daily for five days, with Merck’s being four pills each time and Pfizer’s being three pills each.
There is also remdesivir, an intravenous medication that must be started within seven days of COVID symptoms appearing.

In this photo illustration, a box of Pfizer’s Paxlovid is displayed, July 7, 2022, in Pembroke Pines, Fla.
Joe Raedle/Getty Images
“I do think that we don’t necessarily make use of the tools that we have on hand in the best way possible,” Moody said. “I’ve certainly talked to people who have gotten medications when they got COVID and they made a huge difference. … The trials’ data would definitely suggest that the drugs are effective.”
“I do think that we may not be using the drugs as effectively, or in as many people as it might help,” he continued.
Moody said it’s possible some COVID patients are coming down with symptoms but are not going to the doctor until their symptoms become severe. Alternatively, some people are not undergoing COVID testing when they have symptoms and, therefore, are missing COVID diagnoses.
“I’m sure that there are people who are infected who are not being detected [and not being] treated,” Moody said, but he added that not everyone needs to be tested regularly and that just high-risk people should test more frequently.